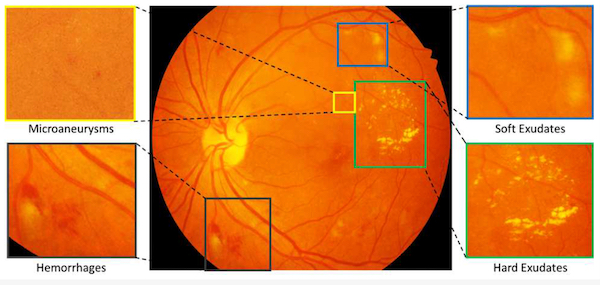
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina, the part of the eye that is responsible for vision. Over time, high blood sugar levels can damage the blood vessels in the retina, causing them to leak fluid or blood or become blocked.
In the early stages of diabetic retinopathy, there may be no noticeable symptoms. However, as the disease progresses, it can cause vision problems such as blurred or distorted vision, floaters, and even blindness if left untreated.
There are two main types of diabetic retinopathy: non-proliferative and proliferative. Non-proliferative diabetic retinopathy is the milder form, where the blood vessels in the retina become damaged and leak fluid or blood. Proliferative diabetic retinopathy is the more severe form, where new blood vessels grow abnormally in the retina, which can cause bleeding and scarring.
Diabetic retinopathy can be diagnosed through a comprehensive eye exam, which may include visual acuity tests, dilated eye exams, and imaging tests such as optical coherence tomography (OCT).
Treatment for diabetic retinopathy may include managing blood sugar levels, controlling blood pressure and cholesterol, laser therapy or surgery, and sometimes injecting a drug (Anti-VEGF) into the eye to prevent or treat vision loss. It is important for people with diabetes to have regular eye exams to detect and treat diabetic retinopathy early, as early detection and treatment can help prevent vision loss.
Dr Sarbjit Singh
